Sleep Growth: A Rested Development Story
Obstructive Sleep Apnea aka Sleep Cardio
I wrote this in March and only got around to editing and publishing it now. That’s a good thing. I didn’t need to change much, but my energies were better spent elsewhere during the intervening months. Allow me to explain.
At the end of February, I got a CPAP (Continuous Positive Air Pressure) machine for my Obstructive Sleep Apnea (OSA), and I’m experiencing restorative sleep for the first time since the womb.
I haven’t been writing since I got the machine. Turns out that getting actual rest allows you to recover much more quickly from…just about everything. As such, I’ve been using this newfound energy to accomplish all the things that have been practically impossible when running on garbage sleep. I’m still playing catch up with sleep, which will probably last until my 70’s. Then I suppose I’ll feel properly rested and finally ready to take on the world.
Drugs
Wrapped up in the topic of my sleep is my stimulant medication. After three years of tinkering, I settled on my ADHD drugs. 50 mg Vyvanse in the morning and 2 mg Intuniv at night. Lock it in.
Glad to be able to close this chapter and reclaim all the brain space that I devoted to the titration process. It’s a major accomplishment whenever I finish any project because of ADHD, and this one was a doozy. One of the reasons I pursued the CPAP so hard was because I was starting to feel like I hit the ceiling with the drugs. Even if I had the stomach for a fourth year of testing drugs, I have a hunch that I wouldn’t get much further with it.
I asked my family doc what was the longest refill he could prescribe for me he could write for both drugs, and he said 3 months. My dosages were already stable for quite a while, so this change in prescription is the final page in the chapter.
Thus, I can finally stop going to the pharmacy every month or so, which has been comically difficult to get to despite my pharmacy being 2 blocks away and doctor’s office being across the street.
This should probably be my last drug update too. Huzzah!
Obstructive Sleep Apnea
I’m gonna (try to) speedrun through the story of how I got my CPAP machine. Not sure if it’s going to be interesting to anyone, but I’ll at least record it for my own terrible memory. Most of you are advised to skip to the next section.
2023 Sleep Study
December (I think). After describing how rough my day becomes whenever I don’t have stimulant meds in my bloodstream, my family doc suggested a sleep study.
Doc: “Do you want to go through the public or private system?”
JL: “Public.”
Surprisingly quick to get the kit from the Foothills hospital. In bed, I hook myself up with a few sensors. Little box sits on top of my little nightstand.
Heart rate monitor on my finger
Oxygen sensor in my nostrils
Breathing monitor strapped around my chest
Accelerometer to detect the angle of my body.
Worst sleep I had in a long time.
Results come back with “possible mild sleep apnea.”
Didn’t hear anything for a while, so called the sleep clinic in July about next steps.
“You don’t need to call us. We will call you when it’s your turn. It will be in the fall.”
Whoa. Attitude.
Waited for the fall call. Nothing, so I dropped it.
“Must not be that bad if they aren’t calling me back. Other people probably need it a lot more than me anyway.”
Thought about that phone call whenever I didn’t sleep well, which was most nights.
Ear, Nose, and Throat (ENT) Doctor
Separately, I had lined up an appointment to see an ENT in June 2024 for allergy concerns.
ENT Doctor: “You probably also have sleep apnea. Have you done a sleep study?”
Me: “Yep.”
“What’s your score?”
“What score?”
“AHI score. Apnea-Hypopnea Index. The number of times you stopped breathing per hour.”
“…”
“…”
“I don’t know. I was just told possible mild sleep apnea.”
(Digging up the results, I now see that the report was quite comprehensive, but very little of it was explained to me at the time. Score was 12.0 per hour. Below 15.0, so mild.)
ENT explained the various treatment options in great detail.
Pharmacotherapy, which is what I’ve already done up to this point. Maybe done the first of five years of allergy serum injections. Daily antihistamines and steroid inhaler until the allergy shots took hold. Drugs already helped a lot, so maybe I didn’t need any further treatment. (Narrator: “He did.”)
Behavioural therapy, like sleep hygiene, meditation, yoga. Tried this for years, never worked, gave up on it forever.
Surgical, like opening my airway, which is pretty narrow for a person my size.
Wait wut. My airway is small? I’d been told that my mouth is (physically) small, but dafuq.
“Yeah, so say you didn’t have sleep apnea. Then at the best of times, your body still struggles to breathe because the pipes are so small. Do you struggle to catch your breath during periods of heightened physical exertion, like playing sports?”
“…A little, yes. I just thought that was normal from being out of shape or not doing enough cardio.”
*she puts a scope in my nose*
Nostrils too small.
Septum deviated, blocking my right nasal passage by about 30%.
“Have you ever noticed how you can breathe better through your left nostril?”
“…”
“Okaaay. Well, have you ever noticed that you sometimes breathe through one nostril and not the other?”
“I thought that was normal.”
“Do you breathe through your nose or mouth?”
“Knuckle-dragging mouth breather.”
“When you pull the skin on your cheekbones apart, can you breathe better through your nose?”
“Yes. Wtf”
Nasal valve has collapsed mildly. Like, the skin on the outside of my nose, below the bridge, isn’t as perky. Normal with age.
*she checks my throat*
Airway opening is reduced by the flaps in the back of my mouth.
Tonsils crowding the back area.
Surgery could provide a minor improvement if I’m willing to endure major pain and a long recovery.
These are her proposed procedures, as I understand them:
Septoplasty with bilateral turbinoplasties - Shaving down my septum for equal airflow between both nostrils.
Columellar rhinoplasty - making my nostrils a bit bigger to improve airflow. Alternative to nasal valve repair but with lower visual impact.
Tonsillectomy - remove my tonsils.
Palatopharyngoplasty - cut my palatoglossal arches and stitch them closer to my cheeks, like opening curtains.
She advises that if I do another sleep study and if it reveals that I have moderate sleep apnea, a CPAP machine would allow me to sleep restfully without the risks of surgery, like infection, pain, recovery time. Surgery could change my voice. My nose will look different. Eating will feel different.
Cut me the hell up. I acknowledge that it seems a tad hasty. I will take the pain. I will accept the new voice and visual updates. I want to breathe.
Sleep is life, and I want to live.
ENT understands that I understand. Still strongly suggests doing another sleep study because that will inform how to proceed with the surgeries. Then we can measure how bad my breathing and sleeping really are.
2025 Sleep Study
Private clinic. For the record, this isn’t an indictment of the public healthcare system. It’s simply the present reality of past budget cuts by conservative governments to starve the beast, all in preparation for private healthcare in Alberta, à la Bill 55.
Score of 16.4. That is, I stopped breathing for 10 seconds or longer at a rate of 16.4 times per hour during my study. My score from the previous study was 12.0. If my score is in the moderate range, then my insurance will fully cover the CPAP machine, along with the mask and accessories. Score of 15 or above is considered moderate severity.
Get set up for my CPAP machine and mask by another technician. She pulls up my study results.
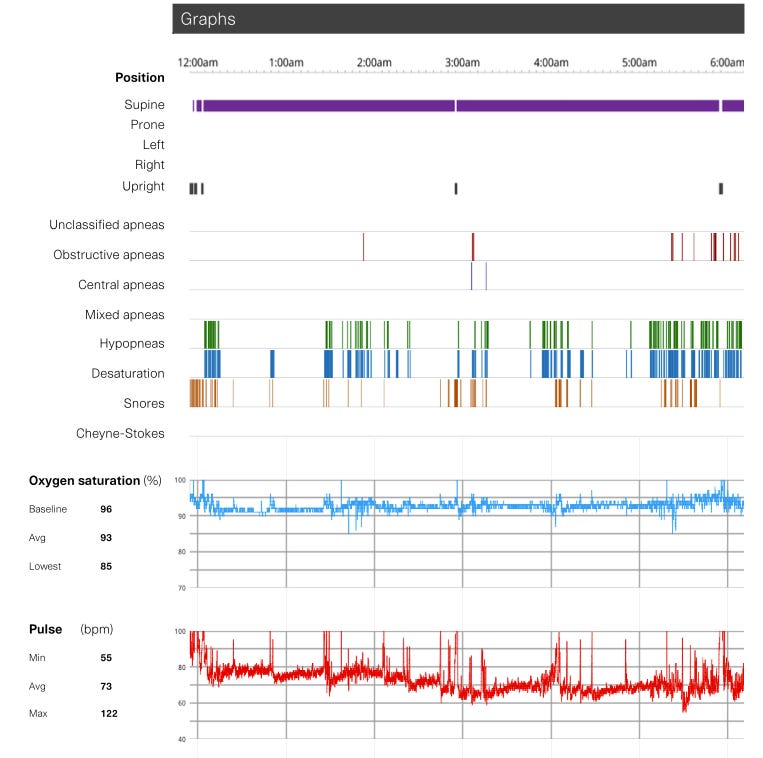
Technician: “See the red graph at the bottom labelled Pulse? It shows your heart rate moving up and down between about 60 and 100 beats per minute.”
JL: *nod*
Tech: “Now look at this graph with the blue line just above it, Oxygen Saturation. When your airway closes, your blood has lower blood oxygen saturation. Makes sense, right? Every time the blue line goes down, the red line shoots up.
“Whenever you can’t breathe in your sleep, your heart works overtime.”
JL: *eyes widen slowly in horror*
Tech: “Your brain needs a consistent supply of oxygen in order to stay alive. So when you stop breathing and your oxygen saturation drops below about 92% on the graph, your heart rate spikes up to 100 bpm in order to deliver that constant amount of oxygen to your brain. And you stopped breathing 16.4 times per hour.”
JL: “…”
Tech: “So when you’re in bed at night, you think you’re asleep, but your body is actually fighting all night.”
“That’s why you feel tired in the morning.”
Kill me now.
Rested Development
Fast forward to today. I’ve used my CPAP machine for a couple months, and I am…at a loss for words. I am both overjoyed and furious. I want to hug someone and also talk to the manager of something.
Nowadays, my AHI score is below 5/hr, according to my machine. Some nights were 0.5/hr.
Pre- and post-CPAP, sleep lasts 6 hours, which is the most surprising result. The upshot is that now I spend a ton more time in deep sleep. I have a couple years of baseline sleep data from sleeping with my Apple Watch, but for simplicity, let’s look at the month before and after.
The time scales are different because I napped more in March.
Oddly, I slept less with the CPAP, but I got better rest because I spent less time awake in bed and more time in deep sleep. Please pay special attention to the 5 AM region on the Feb 2025 chart. Orange means I’m awake. That is where my misery and suffering lived.
It takes a few weeks to adjust to sleeping with the CPAP machine. Your body freaks out the first couple nights, like “what in the flying fuck is this alien latched to your breathing orifice(s)?” You need to wear the mask during the day to train your body to leave it on all night.
After I started using the CPAP in March, average time awake went down to 6% from 11%. Time in deep sleep went up from 11% to 15%. The numbers don’t seem like all the much at first glance, but those 4-5 percentage points, or 30 minutes, mean that my life feels worth living again. It represents how I stopped obsessing about sleep, stopped blogging, and redirected all that time and energy towards all the activities that were effectively impossible to get to before.
It’s my “happily ever after.”
Post-Script
I feel so many things. Grieving the immeasurable losses. Rewinding to so many dark, fuzzy memories in my teen years laying in bed, trying to fall asleep but gasping for air. Wondering if I would wake up the next morning.
The way the CPAP works is by pushing air into the mask, encouraging my airway to open and to let air into my lungs. Some people have just the nose mask, but I have the full face mask because I’m a mouth breather. The full mask gives me mad pimples on my nose, which are scars now. I can feel people staring more intently at my face now.
Trying to think back to the last time when I felt this refreshed, and I’d have to say it was only a handful of times.
CPAPs don’t cure anything, but they’re a great stand-in until I can get my surgeries. My machine is a lot nicer than I imagined. Quiet, small, easy to operate. Came with a neat little carrying case for travel. Doesn’t count against your carry-on or personal item on a plane.
Imperfect lifesaver ☠️🛟
Yes, I did say happily ever after, but what happened to Sleeping Beauty after she married Prince Charming? While I can see how much my life will improve with the CPAP, it can be a pain in the ass.
It’s another set of hard-to-ignore chores. I have to wash the face mask with soap every day to avoid oil buildup, which ruins the seal and irritates the skin. I already have some pretty noticeable scarring on my nose from the pimples I got after the first couple nights.
It has a humidifier tank that needs to be refilled with distilled water every night or two. It has a cellular connection that uploads my sleep data for my clinic and the manufacturer to adjust as necessary.
The hose and accessories need to be cleaned/disinfected weekly. Yeah, that just hasn’t happened. I try my best.
My model, the ResMed AirSense 11 Auto, has an acoustic sensor that can be used to help their research for new features. Essentially a shitty microphone which only benefits the manufacturer. It was turned on by default when I got it. Reading about it on message boards, users did not know that this model shipped with that kind of hardware. From what I understand, since it’s an acoustic sensor and not a microphone, it’s likely not sensitive enough to pick up human speech. It is placed somewhere in the wind tunnel, so it probably only picks up the wind noise. But if it’s so harmless, why opt everyone in by default and hide its existence from users? Shady on multiple counts.
They have a smartphone app, myAir. Indeed, it was useful to calibrate the CPAP metrics against the sleep tracking app I’ve been using for the last few years, AutoSleep. Switching pillows improved all my numbers. Thought I could stop using my mouth guard now that I have the CPAP, but my sleep improved when combining the two, so there we go. However, it’s harder to sleep knowing that there’s probably a shadow network of advertisers tracking not only my sleep but whenever my phone is connected by Bluetooth and therefore my location. Given the shadiness on the hardware side, fair to assume the software is similar. Deleted the app after a few nights since I can just as easily review the numbers every morning on the machine’s little touchscreen. Not sure what the AutoSleep app is doing with my data, but its usefulness is far greater than myAir’s.
My ENT said that based on the initial results of the CPAP and her 20+ years of experience, there was a decent chance that I could be fully cured with the surgeries. At the very least, they’ll improve the effectiveness of the CPAP and could minimize how much or how often I’d need to use it. If I’m okay with the risks, she recommends I follow through because I’m still young. Aiming for November of this year. Can probably take 3 weeks of short term disability because of my insurance.
Overall, I’m overjoyed to have a CPAP machine at all. Got a great machine which insurance fully paid for. The chores aren’t all that bad since my brain is refreshed enough every day that I can prioritize them early. All the negative features of the device can be disabled. Surgery lined up in the same year means all of it feels pretty temporary. Perhaps I can pass on the machine to someone in dire need if/when I’m cured. But one step at a time.
Addendum
Time to play with the words because that’s how my mind works after saying/writing/reading them so often in such a short time.
CPAP. Sleep apnea. Don’t know why they ended up sounding so similar, but whenever I say one of them, people always seem to hear the other. The manufacturer also has a smartphone app that tracks your AHI score every night, a CPAP app for sleep apnea.
If an Atlanta rapper dropped a track on Apnea-Hypopnea, you’d call it hip-hopnea. Or sleep rapnea. A$AP CPAP.